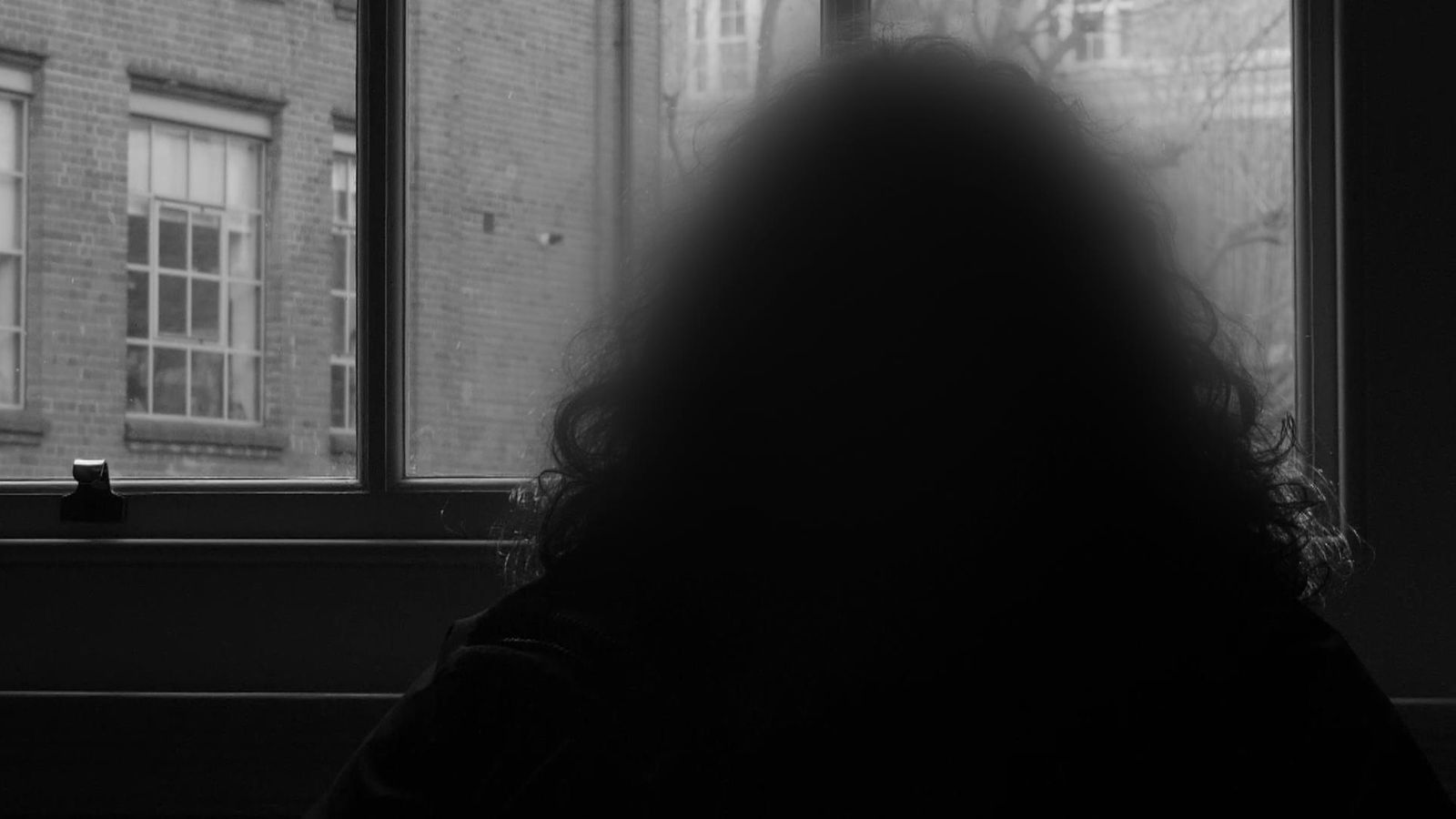
‘It just felt like they’d given up on me’: 30 new patients of Huntercombe Group tell their stories of what life is like at mental health units

Thirty new patients have contacted Sky News following our investigation into the treatment of teenagers in mental health units run by a single provider.
They include a 16-year-old boy whose mother told us her son’s self-harming increased.
Rachel Vickers said of her son Tyson: “He looked like he’d been in a car crash”, and Tyson Vickers added: “It just felt like they’d given up on me.”
In October, Sky News revealed serious allegations of failures in care from more than twenty former patients at units run by The Huntercombe Group, now part of Active Care Group.
Content warning: this article contains references to self-harm
Since then, we’ve been contacted by dozens more former patients independently of one another.
They’ve made further claims over concerns such as the overuse of restraint and inadequate supervision, allegedly leaving patients at increased risk of self-harm.
In response to our joint investigation with the Independent, the Department for Health has described the further allegations of mistreatment as “deeply concerning”.
Sixteen-year-old Tyson Vickers is one of a raft of new patients who’ve come forward in response to our initial investigation.
He spent two months in the Maidenhead unit from the beginning of March this year – he says during his time there he felt “like a lost cause in the mental health system”.
Tyson told us he went into the unit because “I couldn’t keep myself safe”. But he says he didn’t receive the specialist intervention he was expecting.
His mother Rachel said: “I could see that he was getting a lot worse. We were seeing much more self-harm – erratic behaviour that was leading to him needing to be restrained, which we hadn’t had to do at home. It was dawning on me that he wasn’t being looked after.
“He had cuts on his arms. He was bandaged up on both arms. He had a huge black eye. I mean, he looked like he’d been in a car crash.”
Read more:
Calls for ‘rapid’ review of inpatient mental health care following Sky News investigation
Tyson is autistic and transgender. It’s not easy talking about his time at the unit. He said he would ask staff to “refer to me as a male and by the name Tyson with “him” pronouns.
“But sometimes they’d just mess up, and you could tell they didn’t actually respect it”.
Tyson says he gets “flashbacks” from his experiences. He says “just thinking about everything I went through there” makes him tearful when discussing it.
Tyson says: “I was struggling a lot. It just felt like they’d given up on me. I’m not going to get better. I just felt like I couldn’t be helped in any way. I was just sort of like a lost cause in the mental health system.”
“I was told by one staff member I would never get out, that I was just going to be stuck there forever and I couldn’t get help.”
Our original investigation revealed allegations stretching back more than a decade.
There were recurring themes such as the overuse of restraint and lack of staffing and observation to keep patients safe.
The 30 new patients who’ve come forward were inpatients at the units from 2003 – the majority were admitted from 2018.
They all got in touch with us independently of one another.
A patient who wants to remain anonymous, and who was in the Maidenhead unit between 2018 and 2019, told us she is now unable to live independently, which she believes is due to the trauma from her experiences.
This is how she describes her life now after her time at the unit: “I have pretty much daily seizures, walking difficulties, tics and more.
“My mum is my full-time carer as I cannot be on my own due to this. I cannot live independently.”
Another patient, who also wants to remain anonymous, and was admitted to the Maidenhead unit in 2020, shared photographs of injuries to her legs and knuckles which she says were sustained during restraints.
She said: “Sometimes when they were trying to get me in holds, they would swing me round really hard and I would fall into the wall so I would get bruised knuckles.
“Every single day I was getting bruises all over my body.”
Another patient shared pictures she says are of blood on the walls of her room. She told us she was left alone “for hours” to self-harm.
In 2019 Mae, who is 21 now, was an inpatient at Huntercombe’s Stafford unit.
She said: “I wouldn’t be asked to walk to the clinic for a feed, I would just be picked up and dragged there”.
Mae describes feeling like an “animal” in the unit and claims she was “dragged around, locked out of my room, bruised, constantly shouted at and verbally abused.
She said: “I had no autonomy or say in my own care or my own body.”
Ami was in the Maidenhead unit between April 2020 and December 2021.
Now aged 18 she says she wasn’t allowed out of her room for six weeks after an episode of self-harm.
She said when her underwear was taken off so she could be put into anti-ligature clothing, there was a male member of staff in the room.
She said: “I was embarrassed and felt assaulted. It really went past all my boundaries.”
Ami’s mother Rebecca Hinton told us: “We felt helpless, alone, like our voices just fell into a dark well, scared, desperate.”
Separate to our investigation, we’ve learned the first steps have been taken by solicitor Mark McGhee towards legal action against The Huntercombe Group. He’s currently representing nine former patients.
His cases include the family of a young former patient who claims they were raped by a member of staff at the Maidenhead unit.
Thames Valley Police has confirmed they are investigating the allegation.
Mr McGhee said: “This is systemic failure and it’s gross systemic neglect. This hospital was responsible for some of the most vulnerable individuals within our society
“All of these individuals have been profoundly affected in terms of the abuse that they’ve sustained. And it is going to affect the rest of their lives.”
Active Care Group took over Huntercombe in December 2021.
A spokesperson for Active Care Group said: “We are very sad and concerned to hear about these patient experiences and allegations of poor care, a handful of which relate to time in our care…our policies and clinical interventions are in line with national guidelines and best practice; the care of our patients is our top priority.”
“All complaints are investigated and those meeting thresholds for CQC (Care Quality Commission) and safeguarding are reported as required. We are also pleased to receive positive feedback from many young people and their families.”
Read more
‘Blood on the walls’: Investigation reveals the shocking truth behind a children’s mental health unit
‘Treated worse than animals’: Huntercombe investigation reveals decade of mistreatment
The previous owners Elli Investments Group said: “We are saddened by these allegations and regret that these hospitals and specialist care services, which were owned and independently managed by The Huntercombe Group, failed to meet the expected standards for high-quality care.”
NHS England said it’s deeply concerned by these “shocking allegations”.
A spokesperson said: “Consequently these two units, which are run by Active Care Group, have been visited several times by senior commissioners in recent weeks – these visits have included speaking to all current patients, and we will continue to monitor and take appropriate action where necessary.
“The NHS has repeatedly made it clear in recent meetings to the executives of Active Care Group that all services must provide safe, high-quality care and deliver on the commitments in their contracts.”
A Department of Health and Social Care spokesperson said: “The further allegations of mistreatment that have been raised are deeply concerning. Our first priority is to ensure anyone receiving treatment in a mental health facility receives safe, high-quality care, and is looked after with dignity and respect.
Click to subscribe to the Sky News Daily wherever you get your podcasts
“We take these reports very seriously and are working with NHS England and CQC to ensure all mental health inpatient settings are providing the standard of care we expect.”
Chris Dzikiti, Director of Mental Health at the Care Quality Commission (CQC) said: “It is unacceptable for any young person who needs mental health support to receive anything less than the highest standards of care.
“We are grateful to each and every person who has taken the time to share their, or their loved ones, experience of the care they have received.
“We have a range of powers we can use if we find people are not receiving safe care and will take every action possible to protect people where necessary.”